Special section Liver tumors
Definition
Liver tumors are rare in pediatric age group, account approximately 1–3% of all malignant tumors.
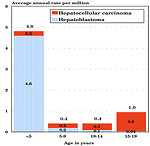
Type of hepatic malignant tumor is age-dependent (Figure 1).
Two-thirds of hepatic neoplasms are malignant (65–75%).
The most common types of hepatic tumors are hepatoblastoma and hepatocellular carcinoma.
The most common benign tumors are vascular tumors (haemagioma, hemangioendothelioma).
Other types of tumors (mesenchymal origin) are extremely rare.
Liver is frequent localisation of metastatic spread of other abdominal pediatric tumors (neuroblastoma, sarcomas, germ cell tumors, lymphomas).
Epidemiology
Liver tumors are the third most common intraabdominal neoplasms in childhood.
Hepatoblastoma is the most common hepatic tumor in childhood, it account > 80% of all liver tumors in children and affects infants and young children ( 6 months – 3 years, median age 19 months). In children over 7 years of the age is rare (Figure 2)
- annual incidence of hepatoblastoma is 1.5 : 1 million
- there are geographic differences in incidence – hepatoblastoma is more common in Japan and Asia than in Western countries
Hepatocelullar carcinoma (HCC) is rare tumor in pediatric population. In adult population HCC is the fifth most common tumor world-wide with incidence 2.4:100 000 and peak age 45–49 years.In population younger than 20 years of the age:
- represent about 0.5% of all cancer in children and teenagers
- ratio HCC : HBL = 1 : 7
- annual incidence of HCC is 0.5 : 1 million, but is higher in countries where endemic hepatitis B infection with its vertical transmission is common (Asia, Africa) (Figure 3)
- HCC is typical liver cancer in adolescent age group, median age at diagnosis is 14 years
- HCC is more frequent in boys
Etiology and etiopathogenesis
Hepatoblastoma:
- etiology is usually unknown, and occurrence is sporadic
- extremely low birth weight (less than 800 grams) is associated with development of hepatoblastoma
- environmental factors (alcohol, drug abuse during pregnancy, motherś hormonal treatment for sterility, maternal occupational exposure to heavy metals, petroleum products and paternal exposure to heavy metals) appear to be risk factors
-
hepatoblastoma may occur in association with variety of congenital anomalies:
- hemihypertrophy (Figure 4)
-
association with genetic predisposition syndromes:
- Beckwith – Wiedemann syndrome
- Gardner syndrome
- Familiar adenomatous polyposis (FAP), risk to develop hepatoblastoma is 1 : 250
Hepatocellular carcinoma:
There are several risk factors causally associated with development of hepatocellular carcinoma:
- chronic hepatitis B and C infection (integration of viral DNA into the hepatocyte, transformation of hepatocyte and cirrhotic changes in liver parenchyma) (Figure 5)
- alcohol and drugs (anabolic steroids) abusus
- exposure to aflatoxins, thorotrast, vinylchloride, pesticides
-
association with a number of underlying chronic liver diseases which develop liver cirrhosis:
- tyrosinemia
- biliary atresia
- neonatal hepatitis
- α1 antitrypsin deficiency
- glykogen storage disease type 1
- Wilson disease
- but 75% of hepatocellular carcinoma in adolescents are sporadic, arising from the healthy liver parenchyma with no cirrhosis or other defined risk factors
Clinical presentation and symptoms
Clinical symptoms depend on:
- size of the tumor
- rapid tumor growth
- age of the patient
- evidence and localization of metastases
The first symptom in both tumors in young age is palpable mass!!!
Hepatoblastoma:
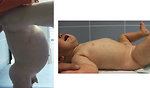
- the first symptom is usually abdominal distension or palpable/visible tumor mass in the right hypochondric area (Figure 6)
- general condition of the child is usually not altered
- child with advanced disease occasionally present with anorexia, weight loss or anaemia
- abdominal pain is present only in case of complications (rupture of the tumor, bleeding and stretching of the Glisson liver capsula )
- jaundice, itching, coagulopathy, edemas or other symptoms of chronic liver failure is exceptional
- sometimes the first symptom is from metastases (10-20%): lungs (cough, dyspnea), brain (seizures, neurological symptoms), bones ( pain), abdominal lymph nodes (palpable mass, ureter obstruction, bowel obstruction)
Hepatocellular carcinoma:
- is asymptomatic for long period of time
- the first symptom – palpable/visible tumor mass (Figure 7)
- later on dominate non-specific symptoms - feelings of fullness and pressure in the abdomen
- anorexia, weight loss, general weakness and fatigue are rare
- symptoms of chronic liver failure are usually not present (no jaundice, ascites, itching)
- exceptionally rarely the first symptom of advanced hepatocellular carcinoma in adolescent age is bleeding from the esophageal varices
Diagnostic procedures
Diagnostic algorithm is identical for both most common liver tumors in childhood.
Family and personal history: doctor has to ask for
- previous pregnancies of the mother, abortions, contraceptives, maternal and paternal occupational exsposure, abusus
- genetic inhereted syndromes in the family, specially FAP
- type of conception ( spontaneous or IVF), pregnancy, birth weight, congenital anomalies, congenital metabolic disorders
- vaccination, infectious diseases ( EBV, hepatitis)
- staying/holiday in the endemic risk areas (Southeast Asia, Africa)
Laboratory tests:
-
hematology:
CBC: paraneoplastic thrombocytosis is common (HB cells secrete IL-1B, which induces fibroblasts and endothelial cells to produce IL-6, which induces hepatocyte growth factor and thrombopoieitin secretion factor) coagulation profile to exclude coagulopathy and deficit of coagulation factors (fibrinogen) - biochemistry: obvious is liver function tests, albumin, ammonia, LDH
- serology: hepatitis A, B, C and virology (EBV,CMV)
-
tumor marker
AFP: is very sensitive tumor marker elevated in 80–90% patients. Serum AFP level has not only diagnostic, but also prognostic significance (AFP negative liver tumors = poor prognosis)
CEA, Ca19-9: in teenagers with liver mass to exclude metastases of the colon cancer
Imaging studies are crucial for diagnosis, initial staging, classification as well as treatment of liver tumors.
- Ultrasound is usually the first test performed. It is non-invasive, give us information regarding primary location of the tumor, helps to evaluate cystic or solid masses, blood supply, tumor thrombus in portal vein (Figure 8)
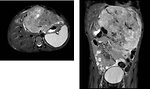
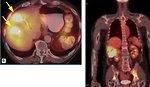
- CT scan: defines tumor extent, relationship to portal and hepatic veins, vascular supply and distant extent of tumor. Initial staging based on initial CT scan – so called PRETEXT classification is mandatory for liver tumor management, plannig surgery as well as prognosis of the patient (Figure 9 a 10)
- MRI: better define tumor relationship to portal and hepatic veins and predict resecability of the tumor (Figure 11)
- 18 FDG PET is not a part of standard work up for liver tumors (Figure 12)
Histopathology
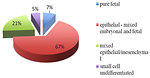
Hepatoblastoma is usually solitary tumor mass, only 20% of hepatoblastomas extend multifocally or infiltrate diffusely into the liver. Hepatoblastoma derived from undifferentiated embryonal tissue/pluripotent hepatic stem cells. Pathological classification is based on degree of differentiation (Figure 13 a 14):
- epithelial type (67%) (mixture of embryonal and fetal type)
- pure fetal type (7%)
- mixed epithelial/mesenchymal type (20%)
- small cell undifferentiated type (SCU, 5%)
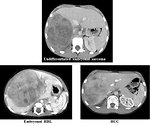
Hepatocellular carcinoma microscopic features of HCC in children are similar to those seen in adults. Pre-existing cirrhosis is present in 5–20% of pediatric patients. Tumor occurs as multiple nodules or a diffusely infiltrating mass (Figure 15).
In adult population the classification of HCC is based on extent of the tumor in liver parenchyma:
- unifocal (single nodule < 5cm)
- multifocal
- diffusely infiltrative type
In pediatric oncology histological variants of hepatocellular carcinoma are important for prognosis (Figure 16):
-
HCC adult type:
- frequently multinodular with extremely invasive growth
- occurs in cirrhotic liver
- vascular invasion and areas of necrosis are frequent
-
HCC fibrolamellar type:
- 30% FL HCC in young people < 20 years
- solitary expansive and excessive mass
- occurs in non-cirrhotic liver
- usually high serum levels of vitamin B12 and transcobalamin I
- AFP could be normal, sometimes gynecomastia
-
Tumor from transitional cells:
- very aggressive biological behavior with poor prognosis
- AFP posit, type between HCC and HBL
Differential diagnosis
In differential diagnosis of liver tumor is important to take into account :
- age of the patient
- character, localization and size of the tumor on imaging studies
The differential balance sheet exclude (Figure 17):
-
other malignant liver tumors:
- angiosarcoma (Figure 18)
- undifferentiated sarcoma
-
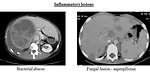
non neoplastic lesions:
- vascular (hematoma)
- inflammatory (abscess bacterial, mycotic, granulomatous) (Figure 19)
-
benign tumors:
- mesenchymal hamartoma
- adenoma, hemangioma
- focal nodular hyperplasia
- teratoma
- infantile hemangioendothelioma
-
metastases to the liver:
- neuroblastoma
- Wilms tumor
- soft tissue sarcomas
- germ cell tumors….. (Figure 20)
Therapy
Surgical treatment
Radical surgical resection is the treatment of choice for both – hepatoblastoma and hepatocellular carcinoma – and is the only chance for cure and survival.
Despite complete surgical resection has been the most effective treatment of liver tumors, less than 50% of liver tumors are resectable at the time of diagnosis (Figure 21).
Biopsy: wedge diagnostic biopsy through a small laparotomy is preferred rather than fine-needle biopsy to confirm diagnosis in both liver tumors.
Radical tumor resection is curative for > 90% hepatoblastomas pure fetal type and is the mainstay of therapy for all other liver tumors.
Factors affecting radicality of surgery:
- size of primary tumor, PRETEXT classification
- localization in the liver, relationship to portal and hepatic veins and hilar structures, therefore is necessary for surgeon to know not only liver anatomy, but he has to be familiar with PRETEXT classification as (Figure 22)
- extraliver disease
Liver transplantation: total hepatectomy and liver transplantation is treatment of choice for patients with multifocal tumor, PRETEXT IV stadium with no extrahepatic disease.
Adult patients indicated for liver transplant must meet Milano criteria (for cirrhotic adult HCC):
- tumor has to be confined to the liver
- non-resectable unifocal tumors (< 10cm in diameter)
-
non-resectable multifocal tumors:
- number of lesions < 5 and
- the biggest diameter < 3cm
- good performance status and function of the liver (Child Pugh criteria)
For pediatric liver tumors in non-cirrhotic liver Milano criteria are not relevant and age specific criteria are not clearly formulated (Figure 23).
Contraindications for liver transplantation:
-
Absolute:
- presence of metastases (even if they disappear after preoperative chemo)
- presence of extrahepatic disease
- presence of macroscopic vascular invasion and/or hilar lymph nodes involvement
-
Relative:
- severe progression of tumor while awaiting liver transplant on waiting list
Chemotherapy
Chemotherapy started to be used in the treatment of hepatoblastoma in late 1980s. Two biggest pediatric oncology groups in a world – COG (Childrens Oncology Group) in USA and SIOP (International Society of Pediatric Oncology) in Europe used different protocols with similar results. Currently international cooperation of both groups as well as national groups of professionals from Germany and Japan working on single protocol accepted worldwide.
Hepatoblastoma
- Is a chemosensitive type of tumor and dramatic improvement of survival has been achieved by implementation of chemotherapy to the treatment
-
Systemic chemotherapy has been used as
-
preoperative ( neoadjuvant ) chemotherapy for initially non-resectable tumors:
- convert inoperable tumor to resectable
- erradicate pulmonary metastases
- eradicate extrahepatic disease
- adjuvant chemotherapy following resection
- palliative for metastatic disease
-
preoperative ( neoadjuvant ) chemotherapy for initially non-resectable tumors:
- Type of chemotherapy depends on hepatoblastoma risk stratification (Figure 24)
Hepatocellular carcinoma
- Is a chemoresistant type of tumor and chemotherapy did not influence overall survival
- Only localized and completely resected HCC is curable
- Advanced HCC is still an incurable disease with poor prognosis
- HCC is phenotypically very heterogeneous tumor with high mutation burden, therefore attention is paid to the new forms of therapy – targeted biology treatment (target angiogenesis, multikinase inhibitors – sorafenib) and immunotherapy.
Locoregional treatment
It is palliative treatment for unresectable tumors which did not meet criteria for liver transplant. Normal liver parenchyma has dual blood supply: 75% from portal vein and 25% from hepatic artery. Liver tumors receive their blood supply almost exclusively from hepatic artery (Figure 25)
Thermoablation: extreme heat destroys cancer cells via laparoscopic procedures
- minimal invasion, less complications
- recovery is usually faster
Limitation for radiofrequency thermoablation is size of the tumor (> 5 cm) and distance from portal and hepatic veins.
Chemoembolization: tiny catether is inserted into hepatic artery, than chemotherapy is injected together with tiny particles to block flow through the artery. Without blood flow drug stays in the tumor area longer. Response rate is 60–80%. Procedure can be repeated several times.
Alcohol embolization is the same principle than chemoembolization, highly concentrate alcohol destroy tumor cells.
Radiotherapy
Radiotherapy is used as palliation for non resectable tumor to reduce its size or to the site of extrahepatic disease for pain control.
Prognosis and outcome
Hepatoblastoma:
Prognostic factors:
- size and localization of the tumor in the liver
- PRETEXT stage
- localized or multifocal liver disease
- age of the patient (less than 1 years and over 8 years)
- rupture of the tumor
- presence of extrahepatic metastatic spread
- initial AFP serum levels
- histological type (pure fetal > epithelial < SCU)
- radical surgical resection
Current 5-year overall survival is > 75%.
Hepatocellular carcinoma
Prognostic factors:
- extent of disease (extrahepatic disease)
- radical surgical resection ( only 30% of HCC is resectable)
- underlying liver disease and liver failure (according to Child-Pugh classification)
- performance status
Compared with hepatoblastoma prognosis is significantly worse.
5-year overall survival is 20–40%.
Author: Viera Bajčiová, MD, PhD