Emergencies in pediatric oncology Hypercalcemia
Definition
Hypercalcemia is defined as serum level elevation of calcium > 2.7 mmol/l:
- serum level of calcium almost always has to be correlate with serum level of albumin
- the key importance is of the free fraction of calcium (ionized calcium), which means calcium not fixed to albumin, the only form that has physiologic effects
- elevated serum level of ionized calcium is > 1.29 mmol/l
Paraneoplastic hypercalcemia is more frequent in oncology of the adult age and may occur in 15–30% of cancer (breast carcinoma, renal carcinoma, non-small cell lung cancer, ovarian carcinoma, multiple myeloma).
In pediatric oncology is paraneoplastic hypercalcemia less frequent, could be associated with rhabdomyosarcoma, neuroblastoma, acute leukemia, malignant lymphoma or Ewing sarcoma.
Pathogenesis
The total amount of calcium in human body is about 1100 g. The skeleton contains 98 % of total body calcium, the remaining 2% circulates throughout the body. One half of circulating calcium is free (ionized) calcium. The remainder is bound to albumin, globulin and other inorganic molecules (Figure 1).
Metabolism of calcium is closely related to metabolism of phosphorus. When serum level of calcium is increasing serum level of phosphorus is dropping down and vice versa.
Homeostasis of calcium in human body depends on several factors (Figure 2). Based on the important function of calcium in the body, level of circulating calcium is strictly regulated by hormones. Parathormon (PTH) is active form of vitamin D (calcitriol, 1.25 dihydroxycholekalciferol) and calcitonin with its effect to the intestine, kidneys and bones maintained stable serum level of calcium (Figure 3).
Cancer may cause hypercalcemia in two ways:
-
paraneoplastic hypercalcemia is caused by
- production of cytokines (cytokines stimulated function of osteoclasts (IL-1, IL-6, TNFα) by tumor itself
- paraneoplastic production of PTH-rP (parathormone related protein). PTH-rP production by tumor is continuous and is not depending on serum levels of calcium. About 80 % of malignant hypercalcemia is cause by tumor production of PTH-rP.
- bone destruction by tumor is caused by primary bone tumor (osteosarcoma, Ewing sarcoma) or metastatic bone lesions with local stimulation and proliferation of osteoclasts leads to bone resorption and osteolysis.
Clinical presentation, symptoms
Clinical symptoms depend on the rate of calcium serum levels increase and the amount of its serum level. It is not clearly known calcium serum level at which the patient begins to have clinical problems. The onset of symptoms is more dependent on the rate of increase calcium levels than the absolute amount of serum calcium. Even relatively high levels may be quite well tolerated, when calcium levels rise in a gradual and slow.
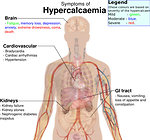
Initial symptoms of hypercalcemia are not specific, started quietly and rising gradually. Unknown hypercalcemia can lead to increasing morbidity and mortality (Figure 4).
- mild hypercalcemia (2.7–3.5 mmol/l) manifests as nausea, vomiting , constipation, abdominal pain and general weakness. Increases the excretion of calcium in urine, leading to failure of kidney concentrating ability, followed by polyuria, polydipsia and dehydration with risk of nephrolithiasis.
- high hypercalcemia (> 3.5 mmol/l) neuropsychic problems occur. During the slow rise of calcium serum levels are mood swings, depressive tuning, headache, hyporeflexia. The rapid increase of calcium serum levels is associated with somnolence, confusion and disorientation.
- very high hypercalcemia (> 4mmol/l) patient is usually unconscious, soporous or in coma. Cardiac symptoms (bradycardia, QT prolongation on ECG, arrhythmia) and cardiac arrest and acute renal failure are imminent (Figure 5).
Diagnostic procedures
Clinical examination can show clinical symptoms of hypercalcemia. It is necessary to monitor clinical status, including state of consciousness (Glasgow coma scale), monitoring fluid balance every 3–6 hours, the patient must be connected to a monitor vital signs (pulse, breath, blood pressure and ECG) at the intensive care unit.
Laboratory examination is crucial for the diagnosis of hypercalcemia - check the serum levels of ions (Na, K, Cl, Ca, P, Mg), glycemia, albumin, renal function tests (urea, creatinine, uric acid) + blood gases. Laboratory parameters must be monitored in 4–6 hours intervals.
Measurement of serum calcium levels must be correlated with serum albumin according to the formula:
Actual serum calcium (mmol/l) = [(40 - albumin) x 0.025] + serum calcium
Measuring levels of PTH-RP did not affect the prognosis and therefore is not routinely investigating.
Imaging studies have no role in diagnosis and management of hypercalcemia.
Therapy
Treatment should be initiated immediately after detection of hypercalcemia simultaneously with anticancer treatment (Figure 6).
- Increased urinary calcium excretion
- Overhydration 3000–4000 ml/m2/day isotonic saline is the first and essential step in hypercalcemia therapy. Hydration filled intravascular volume and enhance diuresis. Do not give intravenously phosphates to the risk of so-called calciphylaxis when calcium-phosphorus product exceeds 70 mg/dl.
- Diuretics need to be indicated very wisely , usually only after hydration, when the patient takes oliguria and fluid retention. Renewed diuresis increases the renal clearance of calcium.
- Diminished bone resorption :
- Bisphosphonates inhibit osteoclastic bone resorption and decrease serum level of calcium. This decline is not fast, calcium level usually decreases after 48–96 hours
- Calcitonin (Miacalcic) is a salmon calcitonin, which inhibits osteoclastic activity. It is well tolerated, it has a rapid onset of effect (12–24 hours), and so is suitable for the acute onset of hypercalcemia. The disadvantage is that it has no long-term effect. In combination with bisphosphonates is useful in life-threatening situations where it is desirable rapid decline in calcium levels. For small children is preferable its intranasal application form, but that is not very effective for hypercalcemia. Therefore it is better to choose the intramuscular or subcutaneous dose of 4–8 IU / kg administered 2 times a day
- Denosumab (human monoclonal antibody) binds to and inhibits receptor activating nuclear factor ƙB ligant (RANKL). Originally it was used for the treatment of postmenopausal osteoporosis and prevention of pathological fractures in bone metastases. May potentially be used for treatment and control of malignant hypercalcemia, which decreases faster and the effect lasts longer than the bisphosphonate.
- Decreased intestinal calcium absorption:
- Corticosteroids via cytokines and prostagladins effect and activate osteoclasts. Corticosteroids also inhibit production of calcitriol and thus have an impact on the reduction of calcium serum levels. Prednison at the dose 2mg/kg/day is usually used.
- Oral phospate in pediatric oncology and pediatric age is rarely used
- Chemotherapy: if hypercalcemia does not exceed a level of 3.5 mmol/l, usually it resolves itself due to anticancer treatment
- Hemodialysis is needed in situation when clinical condition of patient is serious, for patient with renal insufficiency, which is unable to reduce serum calcium.
Prognosis, outcome
Hypercalcemia is the most common life-threatening metabolic complication of cancer patients, although in pediatric oncology is less common than in adults. Late detection can acutely endanger the life of patients, early diagnosis and appropriate therapy results in decreases in serum calcium and elimination of clinical symptoms. Because the symptoms of hypercalcemia are not specific, especially for cancer patient and not arise acutely but gradually increasing, it is necessary to think about this complication and specifically investigate ion levels in the blood and monitor biochemistry and vital signs.
Author: Viera Bajčiová, MD, PhD