Emergencies in pediatric oncology Hyperleukocytosis
Definition
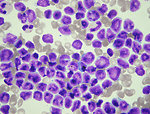
Hyperlekocytosis is defined as total leukocytes count > 100 000/μl in peripheral blood (Figure 1).
9–13 % patients with acute lymphoblastic leukemia present with hyperleukocytosis.
5–20 % patients with acute myeloid leukemia develop hyperleucytosis as presenting feature.
Leukocytosis is presented in nearly all patients with chronic myeloid leukemia.
Leukocytosis is associated with complications: leukostasis and hyperviscosity syndrome.
Pathogenesis
The general principle of leukostasis syndrome is microcirculation thrombotization due to hyperviscosity of the blood. Sludging of circulating leukemic blasts (due to their size and count) causes mechanical obstruction of capillars and consecutive malperfusion in the microcirculation (e.g., in organs such as brain, lungs, renal glomeruli). Apart from the mechanical obstruction, leukemic blasts adhere to the endothelium and interact with it by production of cytokines. These changes after cytokine-driven endothelial cell activation can be a loss of vascular integrity and modification of endothelial phenotype to prothrombotic phenotype. Prothrombotic changes of endothelial cells allow leukemic blasts migration and microhemorrhages (Figure 2).
Leukostasis and hyperviscosity syndrome are more common in acute myeloid leukemia than acute lymphoblastic leukemia. Patients are at high risk of severe life threatening complications.
Clinical presentation, symptoms
Hyperleukocytosis can affect any organ in the body, but usually the first symptoms are related to respiratory system and central nervous system (CSN).
- Pulmonary symptoms: usually started slowly - gradually escalating tachypnea, dyspnea and cough. Leukostasis in pulmonary capillars blocked diffusion of oxygen what leads to hypoxia, acidosis, microthrombotization and bleeding to the lung parenchyma and acute respiratory failure
- CNS symptoms: hyperleukocytosis leads to broad spectrum of neurologic symptoms (headache, behavioral and mental status changes, disturbances of consciousness, confusion, speech problems, ataxia, nystagmus, blurred vision, diplopia, papilledema). There is a high risk of intracranial bleeding.
- Genitourinary symptoms: reduction in renal blood flow and glomerular microtrombotization leads to acute renal failure with oliguria and anuria. Boys may be the first symptom priapism
- Gastrointestinal symptoms: leukostasis in splanchnic vascularization leads to intestinal wall ischemia and bleeding to the intestine. The patient complains of severe abdominal pain plus/minus melena
Clinical presentation of leukocytosis is usually associated with tumor lysis syndrome and syndrome of disseminate intravascular coagulation.
Diagnostic procedures
Clinical examination is focused on examination of peripheral lymphatic nodes (neck, supra and infraclavicular, axillar, inguinal), hepatosplenomegaly, hypertrophy of the tonsils, gingival hypertrophy, skin or mucosal symptoms of bleeding (petechiae). Clinical examination has to confirm/exclude clinical symptoms of hyperviscosity (Figure 3).
Laboratory examination: has a key importance to confirm diagnosis of leukemia and hyperleukocytosis.
- CBC: including microscopic differential count to determine the presence of leukemic blasts in peripheral blood – their character (type of leukemia) and count. CBC usually show hyperleukocytosis, anemia and thrombocytopenia (Figure 4)
- Coagulation profile: to monitor disseminated intravascular coagulation
- Biochemistry: is important for monitoring mineral dysbalance typical for tumor lysis syndrome ( hyperkalemia, hyperphosphatemia, high serum levels of uric acid, LDH), signs of acute renal failure and acido-basic balance
- Monitor of fluid balance (fluid intake and diuresis) and vital signs is mandatory
- Bone marrow biopsy: is essential for confirmation diagnosis of leukemia
Imaging studies: are usually indicated to evaluate complications of hyperleukocytosis
- chest X-ray: is mandatory to see not only lung parenchyma, but also mediastinal lymph nodes. Typical picture of leukocytosis on X-ray is diffuse interstitial infiltrates and mediastinal mass (characteristic for T-cell acute lymphoblastic leukemia) (Figure 5)
- CT scan of the brain: is indicated in case of leukocytosis to exclude intracranial hemorrhage as well as leukemic infiltration of CNS (leukemic plaques or meningeal infiltrates).
Therapy
The main goal of hyperleukocytosis therapy is cytoreduction and decrease blood viscosity to prevent severe complications.
- blood transfusion: must be avoided. Recommended level of hematocrit should not exceed 8–9 gr/dl. Erythrocyte transfusion contributes significantly to serum hyperviscosity.
- hydration: at least 3000ml/m2 iv fluids per day, to maintain diuresis (minimally 5ml/kg/hour)
- specific treatment of leukemia (chemotherapy): is the only causative treatment and has to be start as soon as possible – all other therapeutic options are only symptomatic
- correction of tumor lysis syndrome and DIC: it is recommended to maintain level of platelets > 20 000/μl
-
cytoreduction: indication for cytoreduction depends on number of leukocytes, type of leukemia, age and weight of the child. The key indicator for cytoreductive therapy is clinical condition and symptoms of the child.
- leukapheresis: is a laboratory procedure in which leukemic blasts are separated from the blood. Leukapheresis is indicated for children with body weight over 20 kg. Leukocytes decrease of 50 % is reached by blood exchange of 75ml/kg. Advantage of leukapheresis is rapid decrease of leukocytes. Disadvantage is that this method require special equipment and personnel (Figure 6)
- exchange transfusion: is indicated for young children with body weight less than 20 kg. Recommended volume of the exchanged blood is 150ml/kg. Advantage of exchange transfusion is its simplicity without central venous catheter. Substitution of coagulation factors should be given as well
- supportive care: mechanical ventilation in case of acute respiratory failure and severe hypoxia
Prognosis and outcome
Hyperleukocytosis and hyperviscosity syndrome are the adverse prognostic factors for newly diagnosed leukemias. Patient with hyperleukocytosis is in high risk to develop acute severe life threatening complications:
- hematologic complications – leukostasis, severe disseminated intravascular coagulopathy with risk of intracranial or intrapulmonary haemorrhage
- metabolic complications – acute tumor lysis syndrome and acute renal failure – are common.
Based on literature data hyperleukocytosis is associated with 10–15 % mortality rate in acute or chronic myeloid leukemia and 5% mortality rate in acute lymphoblastic leukemia.
Author: Viera Bajčiová, MD, PhD