Special section Bone tumors Osteosarcoma
Definition
Osteosarcoma is a malignant tumor derived from the primitive mesenchyma of the bone.
Osteosarcoma is characterized by the direct formation of bone or osteoid tissue by the tumor cells.
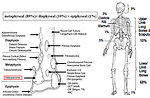
The World Health Organization’s histologic classification of bone tumors separates the osteosarcomas into central (medullary) and surface (peripheral) tumors and recognizes a number of subtypes within each group (Figure 1).
80% of the tumors are localized at the extremities near the end of the long bones (in areas of rapid bone growth) (Figure 2):
- distal femur (52%)
- proximal tiba (21%)
- proximal humerus (10%)
However osteosarcoma can develop in any bone, including bones of the pelvis, shoulder or jaw.
Epidemiology
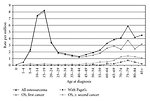
Annual incidence of osteosarcoma is 3.5–5 : 1 million for persons less than 20 years of the age
Osteosarcoma is more common in males than in females, M : F = 1.6 - 2 : 1
It is the 6th most common cancer in children < 15 let and accounts for 5% of all pediatric malignancies
Osteosarcoma can occur in any age, but it is rare in children younger than 6 years
The highest incidence is in the 2nd decade of the life in adolescents between 12 to 20 years and osteosarcoma is the 4th most common cancer in this age group (over 60% of all bone tumors) (Figure 3).
Etiology and etiopathogenesis
Etiology and pathogenesis is usually unknown, most of the osteosarcomas are sporadic.
Some risk predisposition factors are recognized in osteosarcoma:
- Age - modal incidence correlate with teenager growth spurt so it suggest there may be a link between rapid bone growth and risk of osteosarcoma development
- There is known that some genetic diseases and syndromes predispose to develop osteosarcoma based on germline or inherited mutations (Figure 4)
- Benign preexisting bone conditions (hereditary multiple osteochondromas, fibrous dysplasia, enchondromas, localization of bone implants…)
- Paget disease
- Trauma (subclinical trauma – not proven yet)
- Lifestyle related factors have not been linked to osteosarcoma
-
Environmental factors:
- radiation > 20 Gy
- viral etiology (not proven yet)
- chemicals (chlorantheren, AAF, cadmium)
Clinical presentation and symptoms
Local symptoms:
- the first symptoms are frequently underestimated
- pain in the affected bone is the most common symptom of osteosarcoma, initially the pain might not be constant and may be worse at night (on-off pain), later on pain is progressive, particularly with activity
- swelling occur only several weeks after the pain starts, later on is palpable and visible tumor mass, skin over the swelling is shiny with prominent veins, swelling may be worm and tender (Figure 5)
- decreased range of motion in the involved joint, limping
- rarely pathological fracture occur as initial symptom
- lymphadenopathy is unusual
- respiratory findings (cough, dyspnoe, tachypnoe) are symptoms of late disease and lung metastases
Systemic symptoms: fever, weight loss, night sweats are rare and not common
Diagnostic procedures
Physical examination
Physical examination can provide information about palpable mass. Almost always contralateral extremity must be examined with comparison of shape, volume, function of both extremities.
Laboratory tests
Basic hematology exam (CBC, coagulation profile, erythrocyte sedimentation).
Bone marrow biopsy is not a standard part of initial work up.
Biochemistry (urea, creatinine, uric acid, liver function tests, ionogram, CRP)
Non-specific tumor markers: LDH (increased in 30%), ALP (increased in 40%)
Imaging studies
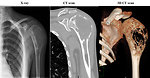
Plain X-ray: is usually the first step, essential for diagnosis is to look for:
- Localization of the tumor
- Margins /limits of the lesion
- Number of pathology bone lesions
- Type of bone destruction (osteolytic, sclerotic)
- Presence of periostal reaction (Codman triangle) (Figure 6)
- Soft tissue involvement
- Relationship to the nearest joint
Plain X-ray of the chest as a part of initial work up is important for diagnosis of lung metastasic spread. It can find larger tumors. If CT scan of the chest is done, a chest-X-ray probably wonť be needed.
CT scan: of the primary localization of osteosarcoma as well as CT of the chest show detailed cross-sectional images of the body (Figure 7, 8).
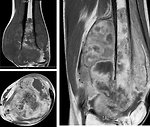
MRI : provide detailed images of the bone, show the exact extent of a tumor as well as detailed view of the bone marrow and soft tissue involvement. Knowing the extent of an osteosarcoma is very important when planning surgery (Figure 9).
Bone scan is an important part of initial work up, it can show the entire skeleton at once. „Hot spots“ on bone scan may suggest skeletal metastases or multifocal bone disease (Figure 10).
18 FDG/PET scan can help show the spread of osteosarcoma to the other organs of the body, but currently is not a part of standard initial work up for osteosarcoma.
Angiography today is not a part of work up, less invasive procedure with the same results is angio CT scan.
Histopathology of tumor tissue: open biopsy must be done almost always in oncology center specialized for musculoskeletal tumors. Biopsy is the only way to confirm diagnosis of osteosarcoma and exclude other malignant bone tumors. The biopsy area including stitch and drain tracks may prove to be contaminated with tumor. The biopsy therefore must be planned so that during definitive surgery the entire biopsy scar can be excised en bloc with the tumor.
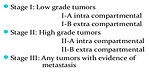
Clinical examination, imaging studies and laboratory results as a part of the initial work up are basic information for initial clinical stage of osteosarcoma. A simple system divides osteosarcomas into 2 groups – localized and metastatic. More than classical TNM staging system for musculoskeletal tumor Enneking staging system has been used (Figure 11).
Differential diagnosis
Factors important for differential diagnosis of bone tumors (Figure 12)
- Age of the patient
- Localization, size and number of the tumor lesions
- Character of the tumor on imaging studies
- Soft tissue involvement
Other bone lesions and diseases have to be distinguished from osteosarcoma:
- inflammatory lesions (chronic osteomyelitis)
- stress fracture
- benign bone lesions (giant cell bone tumor, aneurysmatic bone cyst, osteoid osteoma, eozinofilic granuloma, osteochondroma…..)
- other malignant bone tumors ( Ewing sarcoma, malignant fibrous histiocytoma, malignant lymphoma)
- metastases to the bones (soft tissue sarcomas, renal tumors, neuroblastoma….)
Therapy
Once the diagnosis of osteosarcomaa has been made, a plan of management can be formulated for the particular patient (Figure 13).
Based on chemosensitivity of osteosarcoma and in order to prevent amputation the standard treatment is recommended as follows:
neoadjuvant (preoperative) chemotherapy – surgery –adjuvant chemotherapy
Surgery
The mail goal for the surgery is to safely and completely remove the primary tumor. Radical surgical removal of the tumor is mandatory for survival. The type of surgery depends on the location of the tumor. There are only two options for tumors localized in the arms or legs – amputation or resection and limb salvage surgery (Figure 14):
- Limb salvage surgery have become the standard procedure for almost 94% patients with osteosarcoma. It is very complicated procedure and surgeons must have special skills and experience. Radical resection of the primary tumor has to be followed by reconstructive surgical procedures. The bone that is removed along with osteosarcoma is replaced with a bone graft or with an internal prosthesis made of metal and other materials (Figure 15).
-
Amputation may be the best option for some patients. It involves removal of the limb with a safe margin between the end of the retained portmon and the tumor. Currently only 6% of patients are amputated. Amputation is indicated in case of:
- tumor extends into the nerves and /or blood vessels
- pathological fracture, if vascular and nerve supply is involved
- palliative in case of massive bleeding
- Surgery for non-limbs localized osteosarcoma: pelvic tumors can often be hard to remove with surgery. Hemipelvectomy wih pelvic bones reconstruction can sometimes be done. Tumors of the lower jaw are resected with entire lower half of the jaw and later on replaced with autologous bone graft. Tumors of the spine or skull require combined treatment.
Chemotherapy
Systemic chemotherapy is based on combination of high dose metothrexate, doxorubicin, cisplatin and ifosfamide. All current protocols started with preoperative neoadjuvant chemotherapy with 3 drugs combination followed by delayed surgery at week 10 (Figure 16).
Histological response to neoadjuvant chemotherapy (good responder > 90% of necrosis, poor responder < 90% necrosis) is one of the most important prognostic factors.
Radiotherapy
Radiotherapy has no major role in osteosarcoma treatment. Radiotherapy may be useful in some cases:
- marginal resection of the tumor, where tumor cannot be completely removed (pelvic bones, face…)
- palliation (for pain release, reduction of risk of severe bleeding)
Prognosis and outcome
Negative prognostic and predictive factors:
-
Clinical
- Axial skeleton localization (pelvis, skull, spine)
- Age less than 10 years
- Gender ( boys)
- Size and volume of the tumor
- Spreading to soft tissues
- Metastatic disease: lungs > bone
- Pathological fracture
-
Laboratory:
- Higher serum levels of ALP, LDH
- Higher DNA (hyperdiploid) tumor
- Molecular markers: genetic - RB1 or TP53 germinal mutation, epigenetic- HER2 overexpression, overexpression-P- glykoprotein
- response to neoadjuvant chemotherapy (> 90 % necrosis)
5-year overall survival:
- localized osteosarcoma 65–70%
- lung metastasis (resectable) 55–65%
- non-lung metastasis less than 8%
- local relapse 25%
Author: Viera Bajčiová, MD, PhD