Special section Rare tumors Pleuropulmonary blastoma
Definition
- Pleuropulmonary blastoma (PPB) is a distinctive, rare primary neoplasm of pleuropulmonary mesenchyme occurring in children.
- It is always intrathoracic/intrapulmonary.
- It is categorized into three sub-types (I, II, III), the latter two of which are very aggressive malignancies with metastatic potential. The aggressiveness of PPB appears to progress over time.
Type I, II and III PPB
The PPB Type I, Type II, and Type III are on a biologic continuum:
- Type I PPB is a purely cystic lesion typically occurring in children under 2 years of age, median 10 months of age.
- Type II PPB is a cystic and solid lesion occurring at median age 35 months.
- Type III PPB is a completely solid lesion occurring at median age 41 months.
Signs and Symptoms
Type I PPB
- Mild to sever respiratory distress due to air-filled cysts or pneumothorax.
- Incidental discovery of lung cysts on chest x-ray
Types II and III PPB
- dyspnea, fever, cough, chest or abdominal pain (frequent diagnosis of pneumonia). Respiratory compromise may be extreme with patients on respirators within days of presentation.
- pleural effusion
- pneumothorax (Type II disease)
- malaise, anorexia
Genetics of PPB
Some children with PPB or their relatives (currently estimated to be 40% of PPB cases) may have other cysts or tumor growths. The most common associated problems are:
- multifocal or bilateral lung cysts (sometimes including bilateral PPB)
- benign cystic kidney tumors (particularly cystic nephroma)
- benign eye and nasal tumors
- rhabdomyosarcoma and other soft tissue neoplasms
- benign thyroid nodules or thyroid cancer
- ovarian Sertoli-Leydig cell tumors and dysgerminoma, testicular seminoma, other gonadal germ cell tumors
- leukemias.
PPB appears to have a strong genetic component. Germline loss-of-function DICER1 mutations in 11 families in which there were PPB, lung cysts, cystic nephroma and/or rhabdomyosarcoma. This is the first genetic abnormality described in familial PPB.
Radiographic findings of primary PPB
- benign-appearing cystic lung disease with or without pneumothorax
- partial opacification of a portion of the lung suggesting pneumonia
- complete opacification of the hemithorax
- mediastinal shift and tension pneumothorax
- pleural effusion
- a mass lesion or suggest lobar or larger consolidation
- multiloculated cystic or cystic/solid changes
- PPB involves the lung parenchyma and pleura, but the chest wall peripherally or the mediastinum centrally may be involved as well.
Treatment
Type I PPB treatment
Surgery – is the mainstay of the therapy of Type I PPB. In many Type I cases, the indication for surgery is cystic lung disease and there is little pre-operative concern about a malignancy. Type I disease is entirely cystic and may be unilocular or multilocular, unifocal or multifocal, and unilateral or bilateral. Every attempt should be made to remove completely all cystic remnants to prevent reccurence of PPB. In case of reccurence, Type I recurrences frequently progress to more serious Type II or III disease.
Type II and III PPB treatment
Initial tumor resection is recomended, if it can be accomplished. When this is not possible, open biopsy is recommended. Sites of unresectable residual disease should be titanium clipped for radiographic and possible radiotherapy.
For cases, where initial resection cannot be accomplished neo-adjuvant chemotherapy is indicated. PPB is a chemosensitive disease and response to chemotherapy is prompt, and maximum response occurs after 2 - 4 courses of therapy.
If the patient had a partial resection as initial surgery, 2nd look surgery is recommended and an attempt at complete resection after 2 - 4 courses of IVADo therapy (Ifosfasmide, Vincristine, Actinomycine D, Docorubicine). After definitive surgery and assuming no evidence of recurrence, adjuvant chemotherapy should continue for the another 2-4 IVADo courses.
Radiation therapy
Radiation therapy should be considered for unresectable residual primary disease, after chemotherapy and aggressive attempts at surgical resection.
Author: Pavel Mazánek, MD
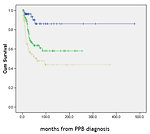 Figure 1: Prognosis significantly differs between al three types (Source - PPB registry). Type I vs II vs III: p < 0.001; Type II vs III: p = 0.029 |
 Figure 2: Plain radiograph |
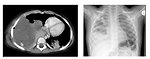 Figure 3: CT scans |
|||||
