Emergencies in pediatric oncology Abdominal emergencies
Abdominal pain in pediatric oncology patient may be caused by several factors, which may be related to the underlying disease or not. Malignant diseases and cancer treatment can affect the abdominal symptomatology several ways - either attenuate symptoms (pain), reduces healing and defense process of the organism and the tumor itself or its treatment leads to the formation of abdominal complications. In about 0.5% to 1.5% of children with cancer develops most frequent acute abdominal symptomatology in childhood - acute appendicitis. Problems with the early detection of signs of inflammation of the appendix may be caused by neutropenia or concomitant medications that may reduce inflammation and this may lead to delay in diagnosis and surgery.
Pathophysiology mechanisms of abdominal emergencies in pediatric oncology are the same as common mechanisms known in general pediatrics – usually it is inflammatory process, mechanical obstruction bleeding or damage of intestinal mucosa with bowel wall perforation and combination of these processes. Significant difference in otherwise healthy child and oncology patient is fact, that process in healthy child is usually localized and in child with malignant disease the same process is usually spread to the whole intestine.
Abdominal emergencies in pediatric oncology could be caused by:
- Tumor itself (B-non-Hodgkin lymphoma, sarcoma etc.)
- Complication of anticancer therapy (surgery, chemotherapy or radiotherapy)
- Not associated with tumor or its therapy (the same risk than otherwise healthy child - appendicitis)
The most frequent abdominal emergencies in pediatric oncology are:
- Enterocilitis necrotisans
- Ileus
Enterocolitis necrotisans
Definition
Neutropenic enterocolitis (NEC) is a serious life-threatening gastrointestinal complication in cancer patients, most commonly occurring in the treatment of hematological malignancies (leukemias and acute non-Hodgkin's lymphomas). This is an acute necrotizing inflammatory bowel disease in children with severe or prolonged neutropenia.
- Typically affects the terminal ileum and cecum (the ileocecal syndrome, typhlitis - from the Greek word typhlon = cecum). NEC defines bowel wall thickening> 0.3 cm on ultrasound or CT scan and the presence of one or more clinical symptoms of suspected NEC.
- Incidence NEC is difficult to define due to broad spectrum of diagnostic criteria, and pathology confirmation of NEC diagnosis is usually missing. According to St Jude Childrens Research Hospital study is incidence NEC in children with cancer about 2.5% , higher incidence is associated with hematology malignancies (leukemias and lymphomas – nearly to 5%). Adolescent patients are at higher risk to develop NEC.
-
Risk factors for NEC development:
- severe neutropenia (absolute neutrophils count < 500)
- mucositis grade IV
- active malignant disease (disease is not in remission)
- malnutrition, catabolism
- poor performance status
- special group of patients – after myeloablative chemotherapy and bone marrow transplantation
Pathogenesis
Pathogenesis of NEC is multifactorial - comprising a combination of damage of the intestinal mucosa by direct toxic effects of chemotherapy, profound neutropenia and insufficient defense of the organism against the invasion of microorganisms into the bloodstream through the damaged intestinal wall (Figure 1).
Any pathogen or intestinal saprophyte could be an etiology agens for NEC. The most frequent pathogens are Clostridium difficile, Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli, Candida and Stenotrophomonas maltophilia.
Clinical presentation, symptoms
Clinical presentation and symptoms are not specific. Diagnosis of NEC is based on clinical trias – abdominal pain, neutropenia and fever.
- Diffuse abdominal pain , abdominal distension
- Water diarrhea (> 80% of patients)
- Intestinal bleeding (melena, hematochesis) depends on severity of mucosal damage ce
- Anorexia, nausea, vomitus
- Symptoms of peritoneal irritation or symptoms of shock (tachycardia, pallor, fever, circulatory instability, hypotension, oliguria igurie) are symptoms of intestinal perforation and peritonitis.
Diagnostic procedures
Physical examination: there is no strict definition of diagnostic criteria for NEC. Common definition of NEC is a case meeting the clinical criteria (clinical trias) and radiology criteria
Imaging studies
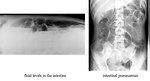
- Abdominal X-ray (both standing and lying position) is a basic examination that demonstrates intestinal pneumatosis, distended bowel loops, subileus or ileus with fluid levels in the intestine (Figure 2).
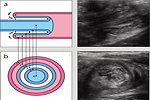
- Ultrasound of the abdomen demonstrated pathognomonic thickening of the bowel wall in the cecum and colon, but also dilated bowel loops, motility, the presence of inflammatory changes in the area of the intestine and the presence of ascites. Ultrasound is a method of choice for children suspected NEC - ionizing radiation does not burden a patient, is well tolerated, is not required sedation, it is painless and can be performed repeatedly on the bed (Figure 3).
- CT scan has a diagnostic value, especially when there is correspondence with the ultrasound image of bowel wall thickening of 0.3 cm. Measurements are performed in both transverse and longitudinal sections of the affected bowel segment (Figure 4).
Laboratory tests: microbial and viral investigations of the blood culture as well as stool. Clostridium difficele toxin plus antibodies in the stool.
Differential diagnosis
- Damage of the intestinal mucosa by primary GIT malignancy - in the ileocecal region mainly non-Hodgkin's lymphoma and neuroendocrine tumors (NET - carcinoid).
- Intestinal form of graft versus host disease (GvHD) after allogenic bone marrow transplantation
- Watery diarrhea as metabolic paraneoplastic symptom of neuroblastoma in infants and/or as a part of carcinoid syndrome in adolescent patients with NETs.
- So called “simple” common infectious diarrhea (clostridium difficile, rotavirus, adenovirus etc.)
- Other inflammatory bowel disease (Crohn disease, ulcerous colitis, secondary malabsorption syndrome).
- Vascular etiology (vasculitis, infarct of intestinal wall)
- Other abdominal emergencies (appendicitis, acute pancreatitis, intususception, ulcerous disease) (Figure 5)
Therapy
Treatment of NEC in pediatric oncology is conservative in most cases.
- antibiotics: neutropenic patient with abdominal symptomatology is candidate for antibiotic treatment in combination with broad-spectrum antibiotics with bactericidal effect on gram negative and gram positive flora (carbapenems, aminoglycosides) and anaerobic microorganisms (vancomycin, metronidazole)
- antimycotics: early indication of empiric antimycotic therapy (amphotericin B ) is at least 48 hours after initiation of antibiotics or in a case of .
- bowel rest and parenteral nutrition: very important is to prevent the most serious complication (intestinal perforation), therefore is recommended no peroral intake (bowel rest), parenteral nutrition with adequate caloric intake to prevent malnutrition and related weight loss
- antiulcerous therapy: antacids and analgesics
- hematologic supportive care: substitution of blood products (platelets, erythrocytes) and/or hematopoietic growth factors (G-CSF).
- surgery: indications for surgical treatment are limited due to successful antibiotic and supportive therapy. The only indication for surgery is perforation of the intestinal wall and uncontrolled bleeding.
Prognosis and outcome
NEC is serious and potentially life threatening complication of anticancer therapy in neutropenic patients. Historically NEC mortality reached almost 80%, currently based on improved supportive care do not exceed 2.2%. Most patients with NEC are managed by conservative treatment without surgical intervention.
Factors with negative impact on duration and severity NEC are prolonged neutropenia grade IV, bowel wall thickening on ultrasound, the presence of peritoneal irritation, the number of clinical symptoms and the patient's age over 16 years.
Author: Viera Bajčiová, MD, PhD
References
1. Bajčiová V: Břišní náhlé příhody. Kapitola 2.5 v Štěrba J a kolektiv: Podpůrná péče v dětské onkologii, NCO NZO Brno 2008, ISBN 978-80-7013-483-2: 53 – 65
2. McCarville MB, Adelman CS, Li CH et al: Typhlitis in chilhood cancer. Cancer 2005; 104: 380–387.
3. Moran H, Yaniv I, Ashkenazi S et al: Risk factors for typhlitis in pediatric patients with cancer. J Pediatr Hematol Oncol 2009; 31(9): 630 – 634.
4. Fike FB, Mortellaro V, Juang D et al: Neutropenic colitis in children. J Surg Res 2011; 170(1): 73 – 76
5. Sundell N, Bostrom H, Edenholm M et al: Management of neutropenic enterocolitis in children with cancer. Acta Pediatr 2012; 101(3): 308 – 312
Ileus
Definition
Ileus is mechanical or adynamic bowel obstruction. In pediatric oncology this abdominal emergency may be caused by either growth of the tumor itself (non-Hodgkin's lymphoma, GIST, bulky tumors of the abdominal cavity) or acute complications of antineoplastic therapy. Ileus may occur in any part of the digestive tract from the stomach to the rectal ampoule.
According underlying cause ileus is divided into 3 groups (Figure 6):
-
mechanical (obstruction): localization may be:
- intraluminal, obstruction is localized inside of intestinal lumen or in intestinal wall. In pediatric oncology the most common cause of mechanical ileus is primary abdominal B- non Hodgkin lymphoma, the most common localization is ileocecal region, neuroendocrine tumors (carcinoid) or soft tissue sarcoma.
- extraluminal, bowel obstruction is caused by compression localized outside of the bowel in the abdominal cavity. Cause is usually intrabadominal tumor (neuroblastoma, germ cell tumor, sarcoma or lymphoma) (Figure 7).
- strangulation ileus is a specific form of postoperative mechanical ileus caused by postoperative adhesions (Figure 8).
-
neurogenic (paralytic): is due to other causes than mechanical. Violation of the signal transmission from the nerves in the intestinal wall musculature leads to muscle adynamia and paralysis. Paralytic ileus may be caused by a single cause, but in pediatric oncology usually several factors are involved in pathogenesis of ileus:
- direct neurotoxicity of cytotoxic chemotherapy: especially vinca alkaloids, sepsis, severe necrotizing enterocolitis and combination of all these factors
- metabolic causes: severe hypokalemia, malnutrition, catabolism
- neurologic causes: spinal cord compression, conus medullaris syndrome
- vascular: failure of blood supply and subsequent ischemia of intestinal wall, either as consequence of thrombosis or embolism in splanchnic blood vessels.
Clinical presentation and symptoms
Clinical symptoms of ileus may begin suddenly or may develop and progress gradually according to the underlying cause.
- Absence of passage stool and gases usually is the first clinical symptom of ileus. Constipation may take several days or may take longer with gradual deterioration. Obviously is associated with abdominal distension.
- Abdominal pain is the principal clinical symptom of ileus. Pain is usually severe, colicky. It may be diffuse (paralytic ileus) or localized (mechanical obstruction). For correct diagnosis is important character of the pain, localization, association with the meal and oral intake.
- Nausea and vomiting: important information is duration of nausea and/or vomiting, allegiance to meal or between meals, vomiting at night. Evidence of blood or bile in the vomit may give us information about localization of intestinal obstruction (small intestine or colon).
- Dehydration important is to measure intake and output of fluids for 24 hours. The amount of urine for 24 hours can help to define grade of dehydration.
- Vital signs changes: tachycardia, fever, hypotension, tachypnea and other symptoms of septicemia
Diagnostic procedures
Physical examination (aspexia) – monitoring of the overall behavior, abdominal distension, respiratory motion waves on the abdominal wall, the color of the skin.
Auscultation informs us of the presence or absence intestinal peristaltics and its distribution. Typical for mechanical ileus are high tones (the sound of falling drops). In paralytic ileus we cannot hear any peristaltics.
Palpation examination must be gentle but precise. We're looking for painful areas of palpation, symptoms of peritoneal irritation or the presence of pathological masses. Digital rectal examination in pediatric oncology has its limitations especially in neutropenic patients (risk of microtrauma of the rectal mucosa and secondary flegmona and septicemia).
Radiology imaging studies significantly contribute to the diagnosis - plain X-ray of the abdomen lying down and standing up, ultrasound and computerized tomography (CT scan) .On the simple image of the abdomen are visible dilatations of bowel loops, with fluid surfaces, uneven distribution of gas in the intestine depends on the localization of obstruction (Figure 9). Ultrasound can measure the thickness of the intestinal wall and consider peristalsis (Figure 10). Abdominal CT scan is helpful in diagnosis of obstruction caused by tumor itself as well as thickness of the bowel wall.
Irigography and colonoscopy is less important in pediatric oncology than in adult oncology due to different types of tumors and therefore different causes of mechanical ileus.
Laboratory studies: Especially biochemical and microbiological analysis is of key importance. Hematology tests - blood count and coagulation profile, as well as biochemical tests - ionogram, liver and renal function tests, markers of inflammation (CRP, ESR, lactate, procalcitonine) are the standard procedures. Crucial part of the investigations is the microbiological surveillance - knowledge of the microbiological colonization of the pediatric cancer patient (all swabs, blood cultures, stool microbiology, perianal swabs).
Differential diagnosis
- Simple appendicitis
- Ulcerous disease with or without segmental intestinal necrosis and perforation
- Simple constipation and meteorism
- Acute pancreatitis
- Enterocolitis necrotisans
- Severe infection (Clostridium difficile, rotavirus, adenovirus, norovirus)
The very important risk factor for outcome is malnutrition, catabolism, severe damage of the mucosal surfaces of gastrointestinal tract, impaired healing after chemotherapy and corticosteroids.
Therapy
Treatment strategy of ileus depends mainly from the underlying cause
- Surgery: in the case of obstructive ileus is the therapeutic method of choice. If the intestinal obstruction is caused by non-Hodgkin lymphoma, the main goal for surgery is to restore intestinal passage and collect material for histopathology.,In a case of paralytic ileus surgery is indicated only in a case of intestinal perforation.
- Hydration and nutrition is important to restore internal environment, electrolytes and energetic supply, usually in form of parental nutrition.
- Antibiotics
- Analgesia: has to be indicated carefully specially before definitive diagnosis of underlying cause of ileus. Opioids may worsen intestinal paralysis.
- Prokinetics: In a case of paralytic ileus caused by vinca alcaloids (with minimal or no risk of bowel perforation) prokinetics are indicated (itoprid, syntostigmin, metoklopramid, erythromycin).
Prognosis and outcome
Intestinal obstruction (ileus) are among acute life-threatening conditions that require rapid detection and adequate treatment. In pediatric oncology are the underlying causes rather than general pediatrics, however therapeutic procedures are not fundamentally different and based on the type of ileus and the underlying cause. Despite progress in modern medicine ileus is still a severe complication of pediatric cancer patients.
Author: Viera Bajčiová, MD, PhD